Impact of COVID-19 on Older Hoosiers
This research brief discusses the risk in older adults for severe illness from COVID-19, hospitalization and mortality rates and the disproportionate impact of COVID-19 on residents of long-term care facilities and people of color.
Key findings include:
- The risk of severe illness, hospitalization, and death from COVID-19 increases with age; and with certain medical conditions common to older adults (e.g., lung disease, heart conditions, and obesity).
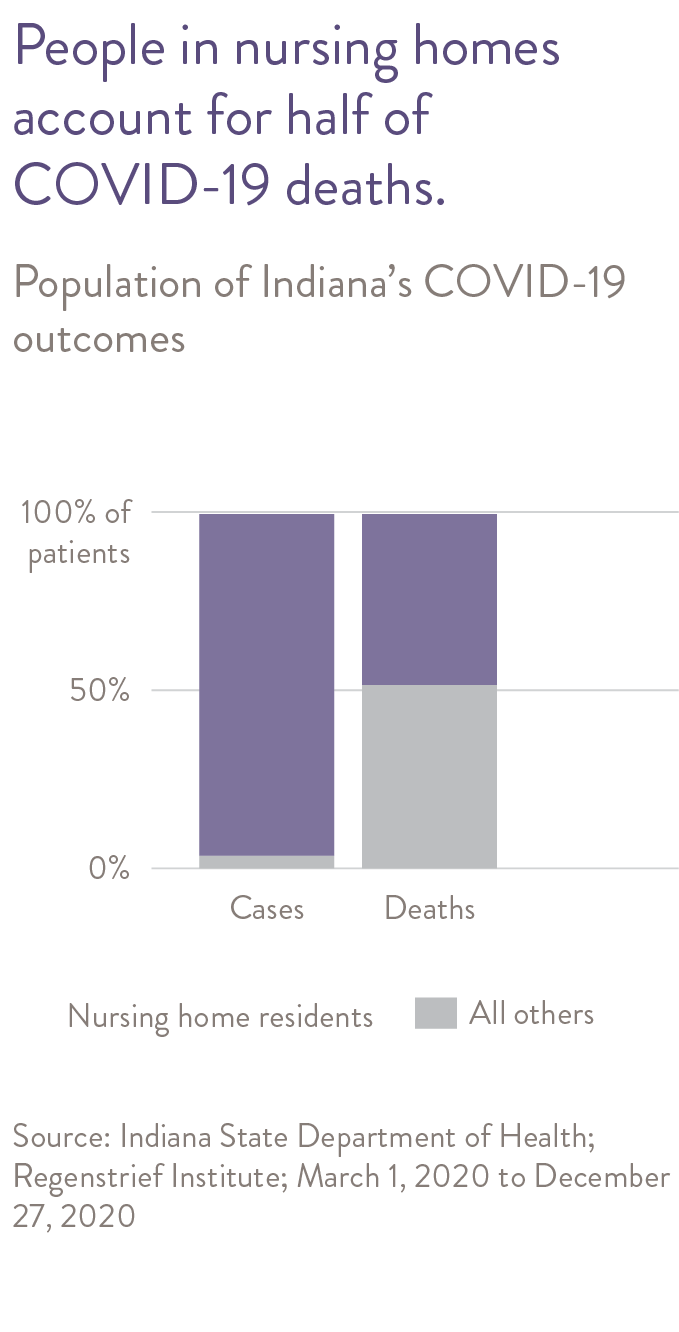
- Nursing home and assisted living residents have accounted for only 4% of confirmed cases but more than half (53%) of Indiana’s COVID-19 deaths.
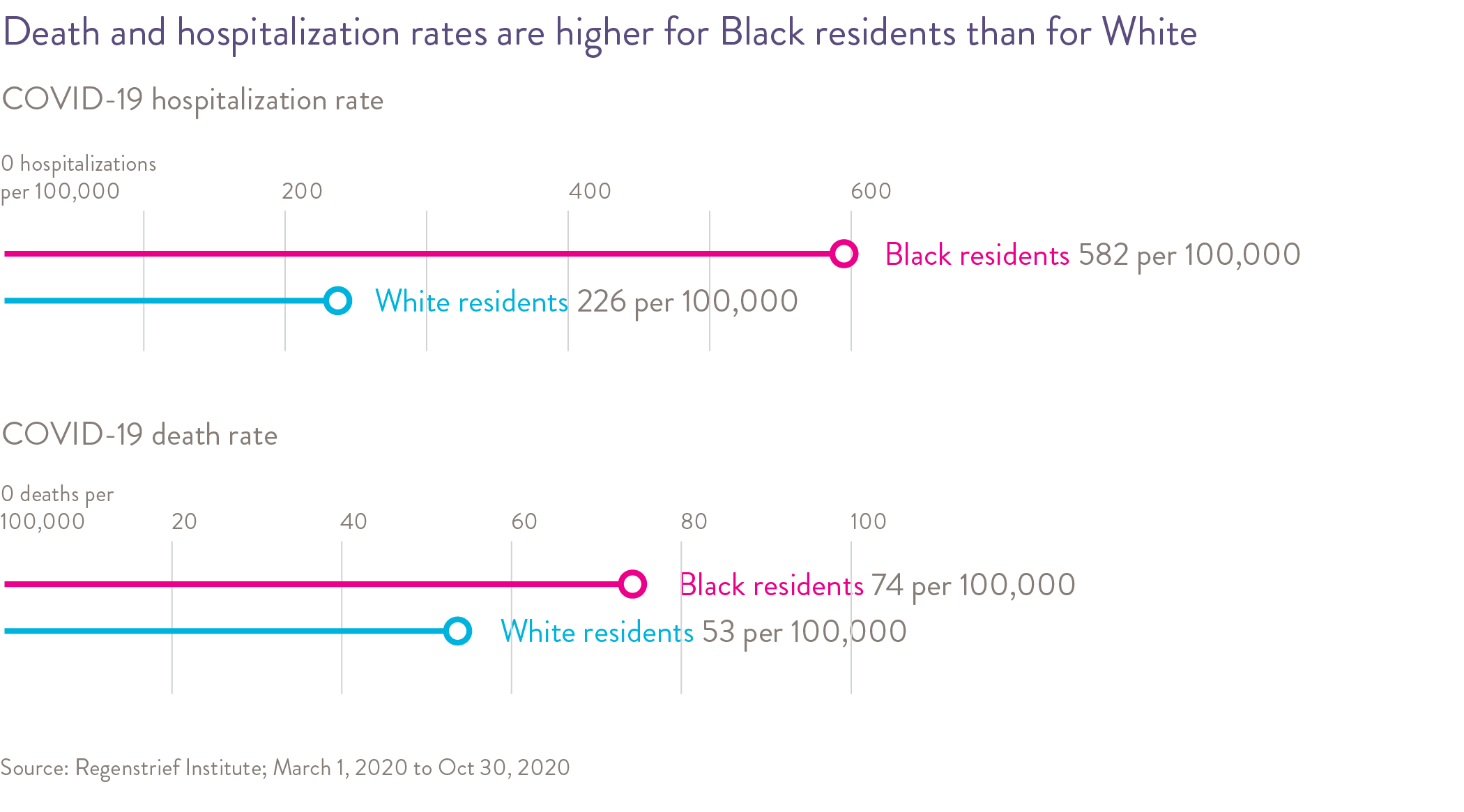
- Available data has shown that people of color have experienced a disproportionate burden of COVID-19 cases and deaths.
- COVID-19 has led to dramatic changes in healthcare delivery including the rapid expansion of telehealth services.
Data Timeline
March – October 2020 for Hospitalization Data
March – December 2020 for COVID-19 Death rates unless specified otherwise
This brief is also available as a PDF.
Indiana’s first case of a person infected with SARS-CoV-2, the virus that causes coronavirus disease (COVID-19), was reported on March 6, 2020 in a Marion County resident. By the end of December 2020, Indiana had exceeded 500,000 confirmed cases and attributed over 8,000 deaths to COVID-19. Central Indiana’s eight of Indiana’s 92 counties accounted for a sizable proportion of these confirmed cases and deaths (20% and 23%, respectively).
Older adults are at particular risk of developing severe illness from COVID-19 such as requiring hospitalization, intensive care, a ventilator to help them breathe, or dying from the disease.
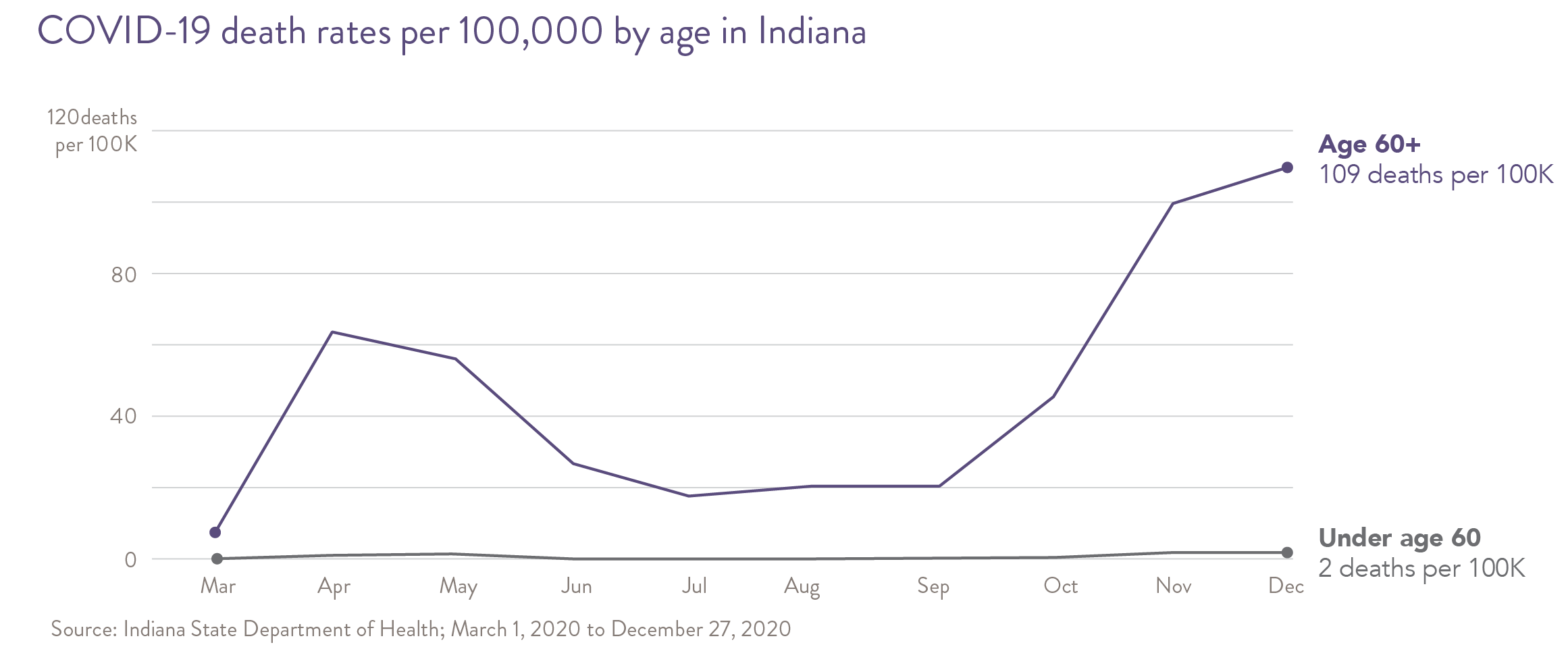
The risk of severe illness increases with age, with older adults at highest risk. People in their 60s or 70s are at higher risk than people in their 50s, and those aged 85 or older are at greatest risk. In addition to advanced age, certain medical conditions increase the risk of developing severe illness from COVID-19. These include cancer, chronic kidney disease, chronic obstructive pulmonary disease (COPD), heart conditions (e.g., heart failure, coronary artery disease) and obesity.
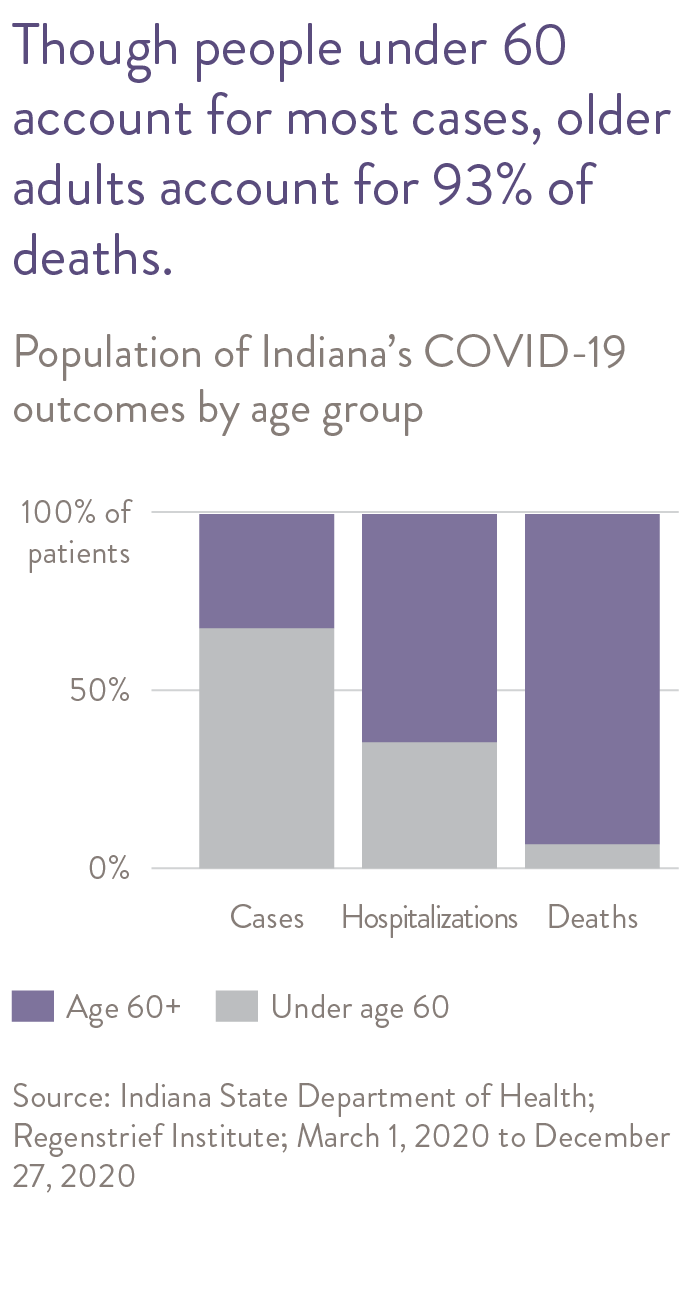
Although rapid advances are being made in the treatment of COVID-19, at the time of this report, approximately 9% of all Hoosiers confirmed positive for COVID-19 were admitted to the hospital. Of those hospitalized for COVID-19 in Indiana, approximately 17% received care in an intensive care unit (ICU) and almost 13% died in the hospital. Although Hoosiers age 60 or older account for approximately 33% of confirmed cases, they account for 64% of hospitalizations and 93% of Indiana’s deaths due to COVID-19.1
COVID-19 in Nursing Homes and Assisted Living Facilities
The situation in nursing homes related to COVID-19 has been referred to as the “perfect storm.” Nursing home residents have an average age in the 80s and most have multiple medical conditions. Furthermore, residents typically share rooms and bathrooms, and receive “high touch” care including assistance with bathing, dressing and toileting, not allowing for social distancing. Many residents with dementia will not tolerate wearing a mask or cooperate with social distancing. Nursing home and assisted living residents in Indiana accounted for only 4% of confirmed cases but 53% of the state’s COVID-19 deaths.
Nursing homes have been severely challenged by the COVID-19 pandemic. Even the best quality nursing homes can have a substantial number of COVID-19 cases and deaths. Studies have demonstrated no relationship between COVID-19 and quality ratings. However, there is evidence that better quality facilities with higher levels of nursing staffing are better prepared to limit the spread of COVID-19 once it is in the facility.
When COVID-19 came to Indiana in early 2020, health care providers made rapid changes in service delivery to lessen the spread of the virus. One of the major changes was the move from in-person office visits to telehealth visits. A national survey of adults ages 50-80 conducted in June 2020 found that in those surveyed, telehealth visits increased from 6% reporting having a telehealth visit prior to March 2020 compared to 26% having a telehealth visit in the period from March to June 2020.2 Telehealth visits were reportedly conducted a third each via video by phone, video by tablet or computer, or by phone with audio only. More than 90% of those that reported having a telehealth visit found it very easy or somewhat easy to use the technology necessary to complete their telehealth visit. Due to the persistence of the COVID-19 pandemic and since older adults will remain at higher risk of severe illness from COVID-19, telehealth visits are likely to further increase and become a standard option for accessing health care.
Racial and Ethnic Disparities
Available data at the time of this report has shown that people of color have experienced a disproportionate burden of COVID-19 cases and deaths. In Indiana, like many states across the nation, Black individuals accounted for more cases and deaths relative to their share of the population. In Indiana, the COVID-19 death rate from March-October 2020 was higher in Black people (74 per 100,000) as compared to White people (52 per 100,000). In general, early national studies have revealed that Black individuals and other people of color were more likely to be positive when tested and have higher rates of hospitalization and death due to COVID-19 compared to White people. In Indiana, the COVID-19 hospitalization rate from March-October 2020 was higher in Black people (583 per 100,000) as compared to White people (226 per 100,000). Underlying disparities such as higher rates of health conditions, barriers to accessing health care and lower incomes and financial challenges put Black individuals and other people of color at increased risk of infection and serious illness due to COVID-19 compared to White people.
- Regenstrief Institute. COVID-19 Dashboard. https://www.regenstrief.org/covid-dashboard/
- Buis, L., Singer, D., Solway, E., Kirch, M., Kullgren, J., & Malani, P. (2020). Telehealth Use Among Older Adults Before and During COVID-19 (University of Michigan National Poll on Healthy Aging, p. 4). University of Michigan. http://hdl.handle.net/2027.42/156253
